“I’m being treated for C. diff colitis that I got after a course of antibiotics for appendicitis. Will it come back? Can my family catch it from me? What’s a fecal transplant?”
Claustridium difficile infection (CDI), or C. diff colitis as it is most commonly called used to be a relatively uncommon occurrence; but, has unfortunately become one of the most common hospital acquired infections world wide. The most common cause of CDI is the prior use of an antibiotic, up to six months ago; however, advanced age, a weakened immune system (chemotherapy), Inflammatory Bowel Diseas (IBD), and the use of Proton Pump Inhibitors (PPIs) like Prilosec have been implicated.
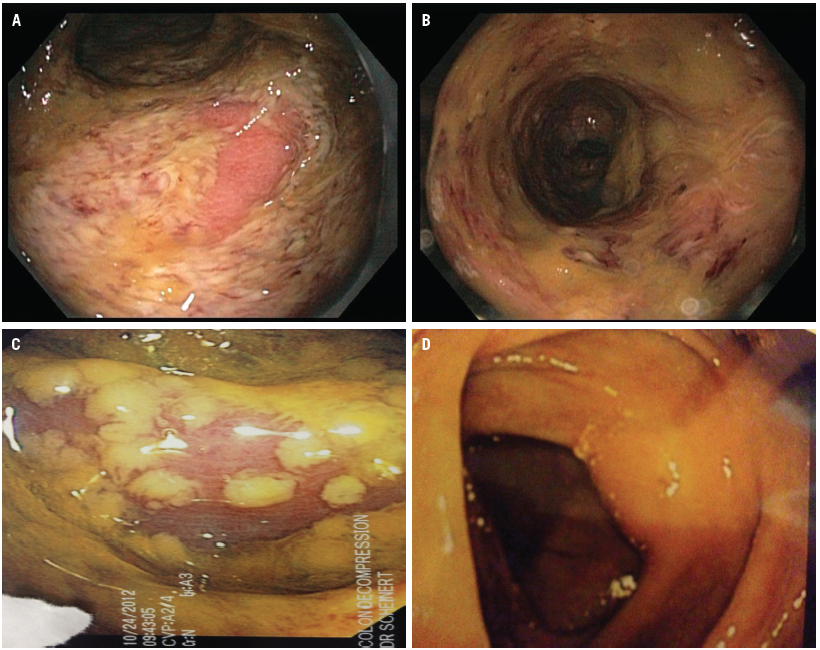
If you have CDI, it is obvious due to the primary symptoms of watery diarrhea (>3 stools a day for > 2 days) and crampy abdominal pain. More severe cases are associated with mucus and blood in the stool, increased pain, and fever. Severe cases are a surgical emergency and if not treated in a timely infection could result in the removal of the colon…and worse.
CDI is caused by broader-spectrum antibiotics effective against gram-negative organisms that normally populate the gut; antibiotics such as (not inclusive) Bactrim, Cipro, Augmentin, Cephalosporins. It is treated by a more specific antibiotic, specific for the C. diff organism, Flagyl or Vancomycin.
It’s not so much the risk of your CDI coming back as it is of it never going completely away as up to half of recurrences are reinfections of the original strain, so it is important to complete the standard course of treatment and to not stop your medication as soon as the symptoms resolve.
Recurrence is defined as a complete resolution of symptoms after treatment, followed by recurrent symptoms, usually within three weeks after stopping treatment, so if you’re out a month, you should be home free. The risk of recurrence is about 25%, likely more in those patients with additional risk factors (see above).
Although it is possible to “give” CDI to your family, it is unlikely in the normal healthy adult or child; however, an elderly parent, or friend or family member on chemotherapy is another matter. Regardless, you must bear in mind that it is spread from hand to mouth, or to put it less delicately, fecal to oral. Of course this means that hand washing is paramount, especially after doing the business and prior to eating and meal preparation.
Lastly, it is quite unlikely you’ll need a fecal transplant—Fecal Microbiota Transplant (FMT); but, they do seem to work nicely. Technically, all you need is someone you trust, water, a blender, and an enema bag, although swallowing would be nearly as effective; however, do not try this at home.
Fecal transplants have been performed for over a hundred years, in cattle; and the first human fecal transplant was performed in 1958, but has not been more widely accepted until the last decade or so.
and the first human fecal transplant was performed in 1958, but has not been more widely accepted until the last decade or so.
The treatment algorithm for FMT generally involves different antibiotics with higher or more frequent doses for the first and second recurrence, and then consideration for FMT with the third recurrence.
FMT is highly effective. It works greater than 90% of the time. Currently, the standard delivery of normal, healthy gut flora (feces) to a sick colon is via a colonoscopy with lavage of the enteric solution throughout the colon. The, ahem, specimen is collected by a lab and then frozen for future use when it is shit, I mean shipped to the end-user, where it is thawed prior to installation. It can also be delivered by an enema, but this is not as effective; and, more recently, pills (30 pills over two days) have demonstrated some efficacy.
Hippocrates thinks it unlikely you’ll suffer recurrent CDI if you take all of your antibiotics for the prescribed length of time. In the unlikely event of a relapse, your doctor will give you different antibiotics, so don’t pull the Ninja from your appliance garage just yet:–leave that to the experts–although, some don’t. Gulp!
Oh, and wash your hands, and use the wipes at Walmart for the bacteria-slimed shopping cart handles.